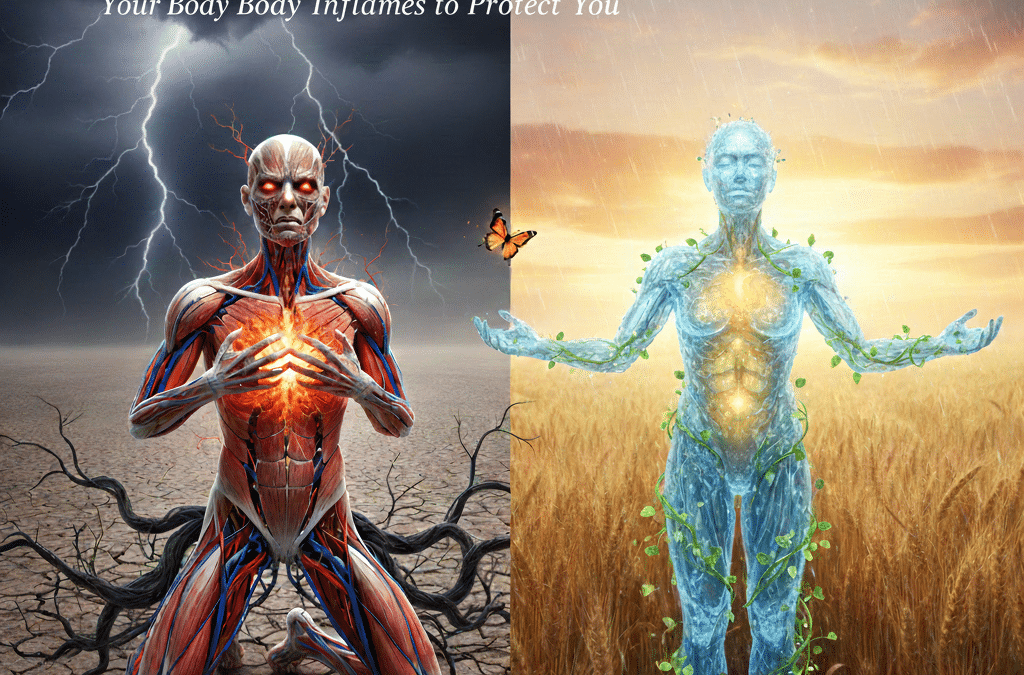
Inflammation is often treated like an enemy — something to suppress, fight, or eliminate. We’re taught to chase it away with medications, supplements, or restrictive protocols.
But inflammation is not the problem.
It is the message.
From a nervous system and fascial perspective, inflammation is one of the body’s most intelligent responses to prolonged stress, threat, or overload.
What Inflammation Is Actually Trying to Do
Inflammation is a protective process. It increases blood flow, brings immune cells to affected areas, and initiates repair. In the short term, it’s essential for healing.
The issue arises when inflammation becomes chronic.
Long-term emotional stress, unresolved trauma, environmental toxins, sleep disruption, and nervous system dysregulation keep inflammatory pathways turned on long after they’re needed.
Research shows that chronic stress increases cortisol and inflammatory cytokines, which directly affect tissue quality, immune signaling, and pain perception.
The body doesn’t forget how to heal — it simply doesn’t receive the signal that it’s safe to stop protecting.
The Role of Fascia in Chronic Inflammation
Fascia is one of the most inflammation-sensitive tissues in the body.
It is collagen-rich, highly innervated, and deeply involved in circulation and lymphatic flow. When fascia becomes restricted or dehydrated, blood flow decreases, lymph stagnates, and inflammatory waste products linger longer than they should.
Studies show that:
- Fascial thickening correlates with chronic pain and inflammatory conditions
- Reduced fascial glide increases pain sensitivity
- Poor circulation in fascial tissue prolongs inflammatory responses
This helps explain why inflammation often presents as:
- Stiffness that’s worse in the morning
- Pain that moves or migrates
- A sense of heaviness or swelling
- Muscle tightness without injury
- Fatigue that doesn’t resolve with rest
Inflammation is not isolated — it’s systemic.
Stress, Safety, and the Immune System
The immune system takes cues from the nervous system.
When the nervous system perceives ongoing threat, immune signaling shifts into a defensive posture. This increases inflammatory output, even in the absence of infection or injury.
From a biological standpoint, this makes sense. If the body believes danger is present, it prepares for damage.
But when stress becomes the baseline, inflammation becomes the baseline too.
This is why inflammation often accompanies anxiety, burnout, grief, mold exposure, Lyme-related symptoms, and chronic illness. These are not separate issues — they are interconnected systems responding to prolonged load.
Why Suppression Alone Isn’t Root-Cause Healing
Anti-inflammatory interventions can be helpful. They reduce symptoms and create temporary relief.
But if the nervous system remains dysregulated and fascia remains restricted, the inflammatory cycle often returns.
Root-cause healing asks a different question:
What is keeping the body in protection mode?
Until that question is addressed, inflammation continues to act as a signal flare — asking for regulation, not suppression.
Supporting Inflammation Through Nervous System Regulation
Research increasingly supports approaches that reduce inflammation by addressing nervous system state and tissue health.
Interventions that improve circulation, tissue hydration, and parasympathetic activation help signal safety to the body. When safety increases, inflammatory signaling naturally decreases.
Low-frequency vibration has been shown to improve lymphatic movement and reduce muscle tension, indirectly supporting inflammatory regulation. Gentle heat increases blood flow and tissue elasticity, allowing inflammatory byproducts to clear more efficiently. Light-based therapies support mitochondrial function, which plays a role in immune response and tissue repair.
At True You Collective, these modalities are used not to “fight inflammation,” but to support the conditions that allow the body to regulate itself.
Inflammation as Communication, Not Failure
One of the most important shifts in healing is reframing inflammation as intelligence.
Inflammation is the body saying:
- “I’m overwhelmed.”
- “I need support.”
- “I haven’t felt safe in a long time.”
This perspective removes shame from symptoms and restores agency to the healing process.
The body is not betraying you.
It is protecting you the best way it knows how.
What Happens When the Body Feels Safe
When the nervous system begins to regulate and fascia softens, several things happen naturally:
- Circulation improves
- Lymphatic flow increases
- Stress hormones decrease
- Pain sensitivity reduces
- Energy returns
- Inflammatory markers begin to normalize
These changes are not forced.
They emerge as the system recalibrates.
This is why many people experience gradual, sustainable improvements rather than dramatic overnight shifts. The body heals in layers — not shortcuts.
Listening Before Fixing
Root-cause health doesn’t ask how fast symptoms can disappear.
It asks what the body needs to stop signaling distress.
Inflammation invites us to slow down, listen, and support the deeper systems at play — fascia, nervous system, circulation, and emotional load.
When those systems are addressed, inflammation no longer has to shout.