For years, fascia was dismissed as “just connective tissue” — something surgeons cut through to get to the important parts. But modern research tells a very different story.
Fascia is not filler.
It is not passive.
And it is absolutely not separate from your nervous system.
In fact, fascia may be one of the most important — and overlooked — systems influencing pain, stress, emotional regulation, and chronic symptoms today.
What Is Fascia, Really?
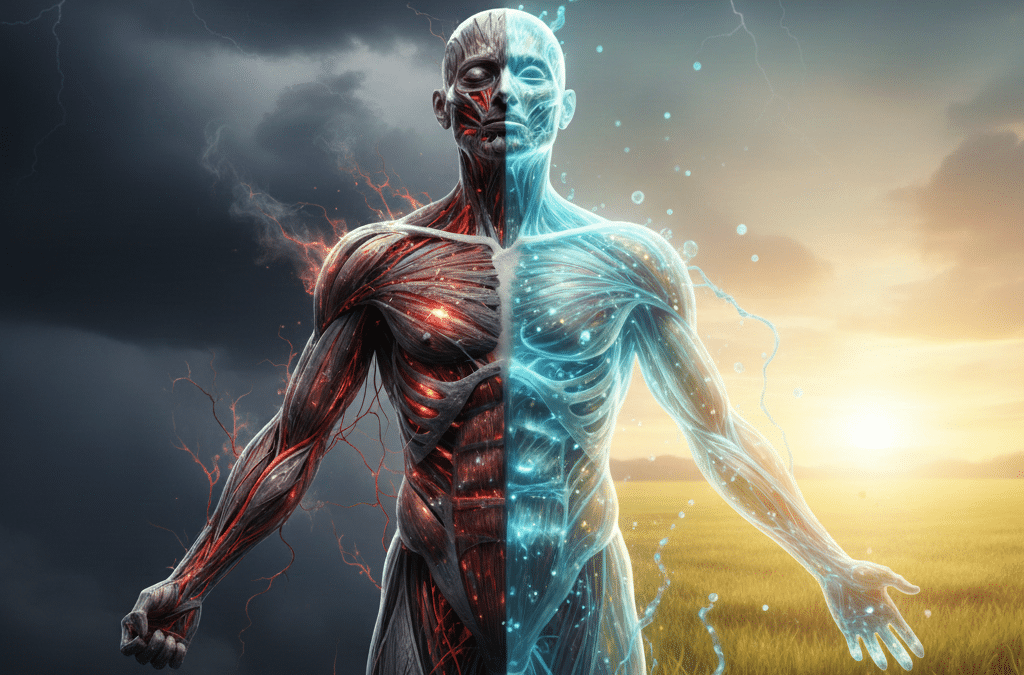
Fascia is a continuous, web-like connective tissue that surrounds and penetrates everything in your body — muscles, bones, nerves, organs, blood vessels, and even cells.
Rather than isolated parts stacked together, the human body is organized as one interconnected tensional system, with fascia acting as the communication matrix holding it all together.
Research has shown that fascia contains six to ten times more sensory receptors than muscle, making it one of the body’s primary sensory organs. These receptors constantly send information to the brain about pressure, tension, position, and safety.
In other words, your nervous system is not just listening to your thoughts — it is listening to your fascia.
Fascia and the Nervous System: A Two-Way Conversation
Your nervous system is constantly asking one central question:
“Am I safe?”
Fascia plays a major role in how that question is answered.
When the nervous system perceives threat — physical, emotional, environmental, or psychological — fascia responds by tightening. This is a protective mechanism. It stabilizes the body, limits movement, and prepares for action.
The problem arises when that response becomes chronic.
Long-term stress, trauma, grief, inflammation, illness, or sensory overload can keep fascia in a shortened, dehydrated, and restricted state. Over time, this restriction feeds back into the nervous system, signaling ongoing danger — even when no immediate threat exists.
This creates a loop:
- Nervous system stress → fascial tightening
- Fascial restriction → nervous system hypervigilance
And symptoms emerge.
Why Fascia Matters in Root-Cause Health
Many common complaints share a fascial and nervous system component, including:
- Chronic pain or tension that “moves around”
- Tight chest or shallow breathing
- Anxiety that doesn’t respond to logic
- Morning stiffness or postural changes
- Fatigue that doesn’t improve with rest
- A sense of feeling “stuck” or restricted in the body
These are not isolated issues. They are expressions of a system under load.
Fascia transmits mechanical tension, emotional stress, and inflammatory signals throughout the body. When it becomes rigid or poorly hydrated, circulation decreases, lymphatic flow slows, and nerve signaling becomes distorted.
From a root-cause perspective, this means many symptoms are not problems to be silenced — they are communications from a system that has adapted to prolonged stress.
Why the Body Holds On
One of the most important things fascia teaches us is this:
The body does not hold tension because it’s broken.
It holds tension because it learned to protect.
Fascia adapts to posture, movement patterns, emotional states, and lived experience. Over time, these adaptations become the body’s new “normal.”
This is why telling someone to “just relax,” “breathe deeper,” or “calm down” often doesn’t work. The nervous system cannot shift into relaxation if the fascia is still signaling threat.
Safety must be felt in the tissues — not just understood intellectually.
Supporting Fascia Without Forcing Change
Research increasingly supports bottom-up approaches to nervous system regulation — methods that work through sensation, vibration, warmth, and gentle input rather than conscious effort alone.
Modalities that support circulation, tissue hydration, rhythmic input, and parasympathetic activation can help fascia soften and rehydrate, which in turn changes the signals sent to the nervous system.
This is why many people experience emotional release, spontaneous breath changes, or a deep sense of relief when the body finally feels safe enough to let go — without having to talk or analyze anything.
At places like True You Collective, the focus is not on “fixing” the body, but on creating the conditions where the body can do what it already knows how to do: regulate, release, and repair.
A New Way of Understanding Symptoms
When we understand fascia as a sensory and communicative system, symptoms stop feeling random or personal.
Pain becomes information.
Anxiety becomes feedback.
Tension becomes communication.
This perspective doesn’t dismiss medical care — it expands it. It reminds us that healing often begins not with doing more, but with listening differently.
Fascia is not the problem.
It’s the messenger.
And when we learn how to work with it — rather than against it — root-cause healing becomes not only possible, but sustainable.