Many people understand their experiences logically.
They know they’re safe.
They know the moment has passed.
They know they’re no longer in danger.
And yet their body still reacts.
The heart races.
The breath tightens.
The chest constricts.
The jaw clenches.
The nervous system stays alert.
This disconnect is not a failure of mindset or emotional maturity.
It is biology.
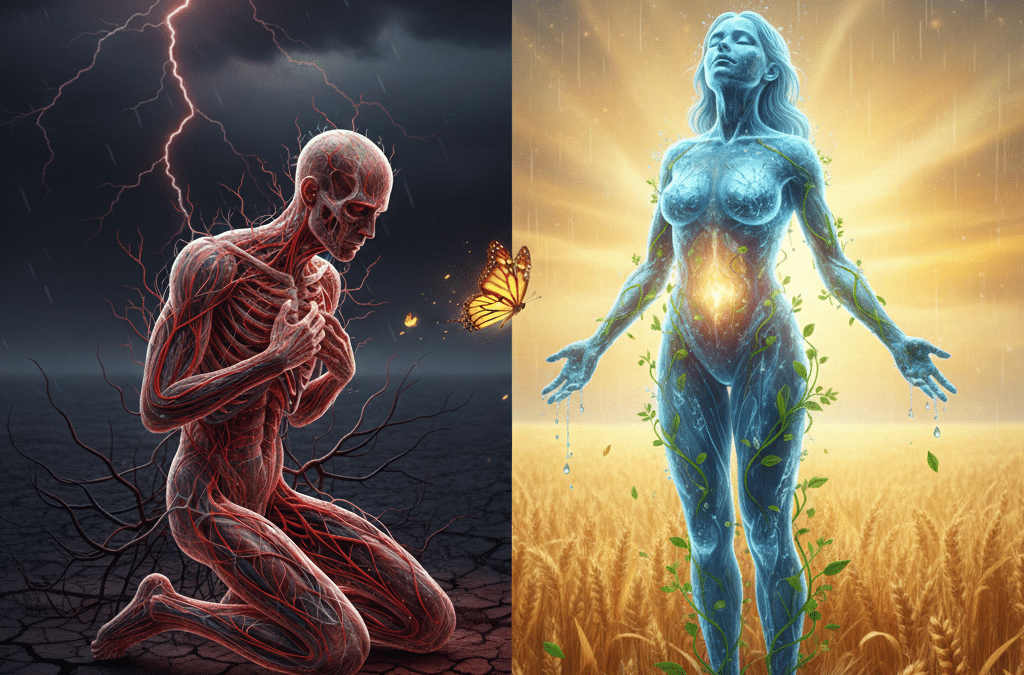
Trauma Is a Nervous System Experience, Not a Memory Problem
From a scientific perspective, trauma is not defined by what happened, but by how the nervous system responded — and whether it was able to return to regulation afterward.
When the nervous system perceives threat, it activates protective responses: fight, flight, freeze, or collapse. These responses are accompanied by physical changes — altered muscle tone, restricted breath, changes in posture, and shifts in blood flow.
Fascia plays a central role in this response.
Research shows that fascia contracts under stress as a protective mechanism. This contraction helps stabilize the body in moments of perceived danger. However, when stress is chronic or overwhelming, fascia can remain in a shortened, restricted state long after the threat has passed.
The body adapts to survive — and then forgets how to soften.
Fascia as a Storage Site for Survival Patterns
Fascia is richly innervated with mechanoreceptors that constantly communicate with the autonomic nervous system. These receptors are sensitive not just to movement and pressure, but to emotional and physiological stress.
When trauma, grief, or prolonged stress occurs, fascia adapts by holding tension patterns that support survival. Over time, these patterns can become the body’s default setting.
This helps explain why trauma often shows up as:
- Persistent muscle tension
- Chronic pain without clear structural cause
- Tightness in the chest, hips, or jaw
- Shallow or restricted breathing
- Heightened anxiety or hypervigilance
- A sense of being “stuck” or disconnected
The body isn’t reliving the past.
It’s maintaining a pattern that once helped keep it safe.
Why Talking Isn’t Always Enough
Cognitive therapies are powerful tools — but they primarily engage the top-down pathways of the nervous system. Fascia and autonomic responses operate largely outside conscious control.
This is why people can talk through experiences, understand their triggers, and still feel physically dysregulated.
Bottom-up approaches — those that work through sensation, rhythm, vibration, warmth, and movement — speak directly to the body’s safety systems.
Research on somatic therapies, rhythmic sensory input, and vagal nerve stimulation shows that the nervous system often needs physical signals of safety before emotional processing can occur.
In other words, the body needs to feel safe before it can let go.
How Sensory-Based Modalities Support Release
This is where research-informed, non-invasive modalities can support nervous system regulation and fascial release.
Low-frequency vibration, for example, has been shown to stimulate mechanoreceptors in fascia and improve vagal tone, helping shift the nervous system out of fight-or-flight. This is one reason vibroacoustic therapy can create deep relaxation without requiring active effort.
Infrared heat supports circulation and tissue hydration, which fascia requires to remain pliable. Heat also reduces stress hormone output, helping the body downshift from protective states.
Red light therapy supports mitochondrial function and cellular repair, which can be compromised under chronic stress and trauma. Improved cellular energy allows tissues to respond more effectively to regulation signals.
Gentle sensory light experiences can influence the brain’s emotional processing centers, helping regulate sensory input without overwhelming the system.
At True You Collective, these modalities are layered intentionally — not to force release, but to create an environment where the body receives repeated signals of safety. Over time, the nervous system learns it no longer needs to hold as tightly.
When Release Happens Naturally
One of the most misunderstood aspects of trauma healing is release.
Release is not something we make happen.
It is something that occurs when the nervous system feels safe enough.
This is why people often experience spontaneous sighs, deeper breathing, emotional waves, or a sense of relief during sensory-based regulation. These are not reactions being created — they are protective patterns being unwound.
The body lets go when it no longer needs to brace.
A Root-Cause Perspective on Trauma Healing
From a root-cause lens, trauma is not about fixing what’s wrong. It’s about restoring what was interrupted: the nervous system’s ability to move fluidly between activation and rest.
Fascia sits at the intersection of this process — amplifying either stress or safety depending on the signals it receives.
When care approaches include both education and embodied regulation, people often find that healing becomes less about effort and more about permission.
Permission to soften.
Permission to breathe.
Permission to stop protecting.
Listening to the Body Differently
Understanding fascia and trauma through a nervous system lens reframes the entire healing process.
Symptoms become adaptations.
Reactions become intelligence.
The body becomes an ally — not an obstacle.
This perspective doesn’t replace medical or psychological care. It complements it, offering a deeper understanding of why healing sometimes requires more than insight alone.
The body remembers how to regulate.
It simply needs the right conditions to feel safe again.